Understanding Food Intolerances
Allergies are on the rise in our society and most people are aware of this: schools are now ‘nut free zones’, the number of allergic kids is growing and in my son’s class last year there was a child who is anaphylactic to dairy, eggs and all nuts! It’s a crazy world we live in.
Whilst allergic reactions to such foods are often obvious and get diagnosed quickly, food intolerances are not as easy to diagnose and are often missed. Food intolerances are responsible for vague symptoms like headaches, behaviour changes such as anxiety/depression, digestive symptoms like IBS (irritable bowel syndrome), aches and pains (including arthritis type symptoms), reflux and indigestion, inability to lose weight and many others seemingly unrelated symptoms.
Why food intolerances matter?
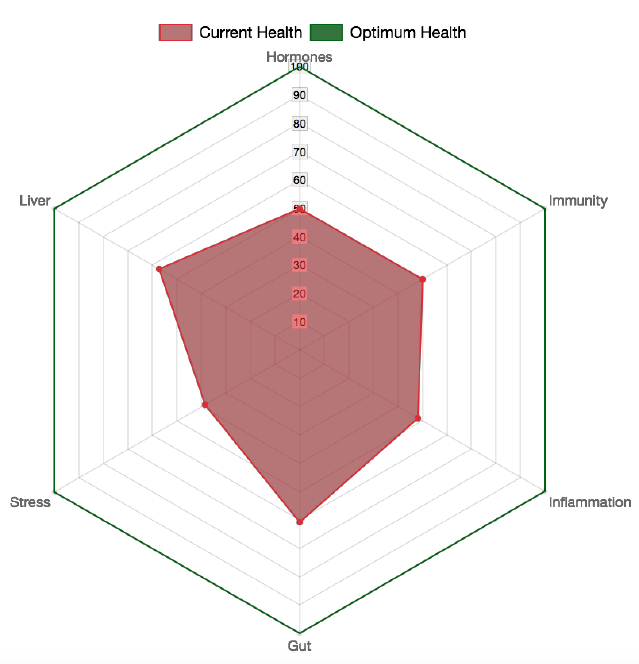
Food intolerances contribute to long term activation of the immune system and undermine health. Continued consumption of foods that instigate an antibody reaction will undermine the immune system over time and contribute to the initiation and progression of numerous health conditions. Researchers have linked numerous disorders to food intolerances. In his excellent article titled ‘Why we get sick and how to get well’, functional medicine practitioner Chris Kresser lists immune dysregulation as one of the keys to disease.
Regularly people use the words allergy and intolerance interchangeably which is confusing and fails to distinguish between these reactions. They are different in the symptoms produced and their effect on health.
Antibodies come in different types
IgE
These antibodies are ‘true’ allergies that involve an immediate reaction via the release of histamine, like rash, swelling, hives, wheezing/asthma, abrupt abdominal pain and diarrhoea upon exposure to a food or inhalant. Often if you do a blood test with your GP you will see ‘Total IgE’ and if there is a number next to it, the antibodies are likely elevated.
If you already know that you are allergic to something (eg: peanuts) and avoid this food 100% but your IgE antibodies still come up, it’s most likely to be environmental allergies like pollens, animal hair, etc. These are the sort of foods commonly identified by ‘scratch’ testing with allergy specialists. These tests do not identify food intolerances.
IgG
These antibodies are the most prevalent in the blood and represent the memory response of the immune system. These antibodies produce a delayed reaction ranging from several hours to several days. These are the types of reactions that most likely you will not ‘feel’, although some people may experience digestive symptoms, headaches and other symptoms described above.
The IgG antibodies form complexes with food particles- they bind to bits of gluten or casein for example- and then land themselves in various parts of the body triggering inflammation. Our immune system will usually ‘deal’ with these complexes however it’s capacity to do so is limited. So if you are continuously eating a food that your body is forming an IgG antibody to, over time the body’s ability to deal with this food is reduced and disease progression sets in.
It is believed that most autoimmune conditions like Rheumatoid Arthritis, Asthma, Eczema, Fibromyalgia as well as headaches, sinus conditions and others begin with food intolerance reactions.
IgA
IgA food intolerance antibodies are similar to IgG as they also show a delayed reaction, but are produced at the gut level, so these are more likely to reflect gut inflammation and show that foods you are reacting to are irritating the gut and triggering the immune response.
A heavy presence of IgA antibodies (as I often see on tests) indicates a compromised defence system at the gut level and shows that intestinal permeability (‘leaky gut’) is present. Research has now shown that autoimmune disease cannot occur without a presence of leaky gut and immune activation.
Why test for food intolerances?
Eliminating foods that your body is producing antibodies to can significantly improve symptoms of numerous health conditions. Testing will help determine whether food reactions are contributing to physical or mental symptoms. It’s also a scientific and reliable way to determine reactions that are difficult to single out even with restrictive elimination diets. Often the foods that come back with high levels of antibodies are foods that the person has been eating for many years without any obvious symptoms. Slowly, these foods are undermining health.
Here is one example of strong food intolerances: this person has not eaten dairy for years as they know they have a strong digestive reaction to it. The memory antibodies (IgG- grey bars) are still there for dairy at low levels. This person is severely intolerant to egg white and moderately intolerant to egg yolk (basically the whole egg!) and has been eating eggs as we all do for their whole life. Finding out that eggs were responsible for several health issues has been crucial to healing.
Grey bars = IgG antibodies, White bars = IgA antibodies
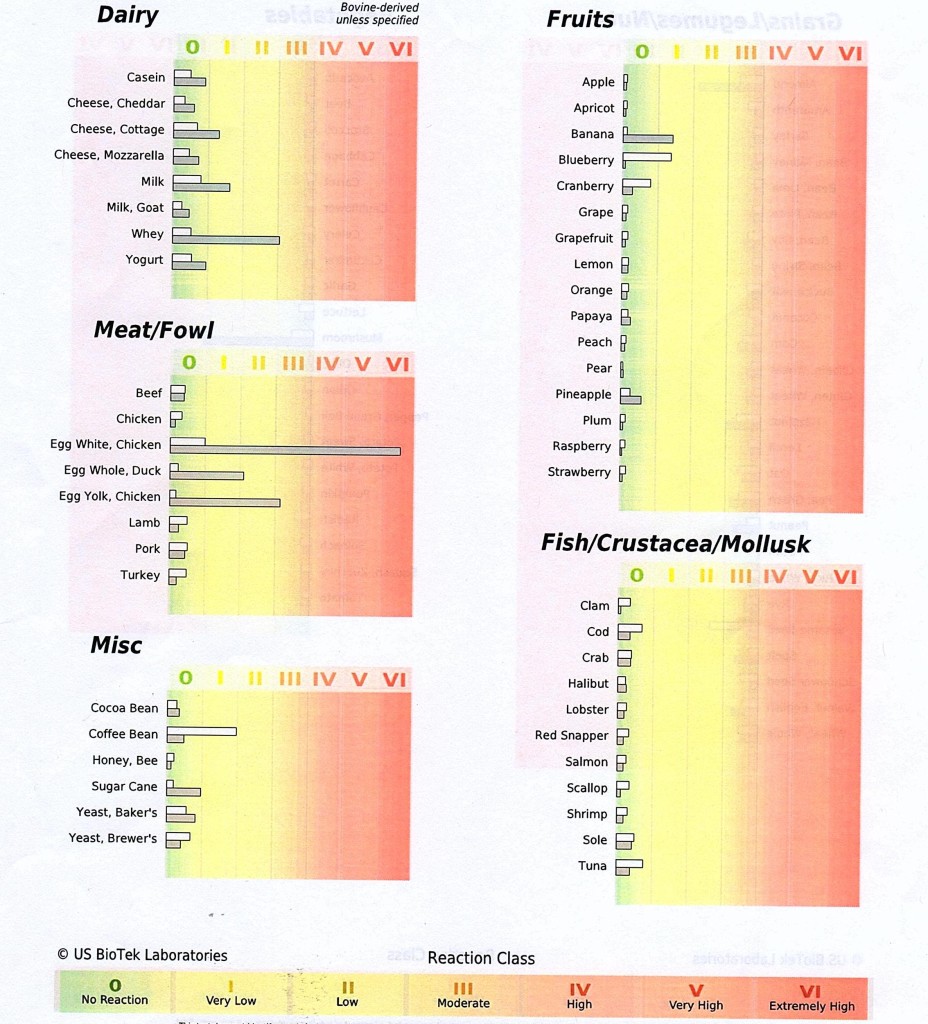
Example IgG & IgA antibody test
Here is another example (different person) of a multitude of antibodies. This person is truly intolerant of wheat and other gluten grains (see grey bars) and has severe inflammatory gut reactions to most other foods including most vegetables. This sort of gut inflammation is at the core of many serious health conditions.
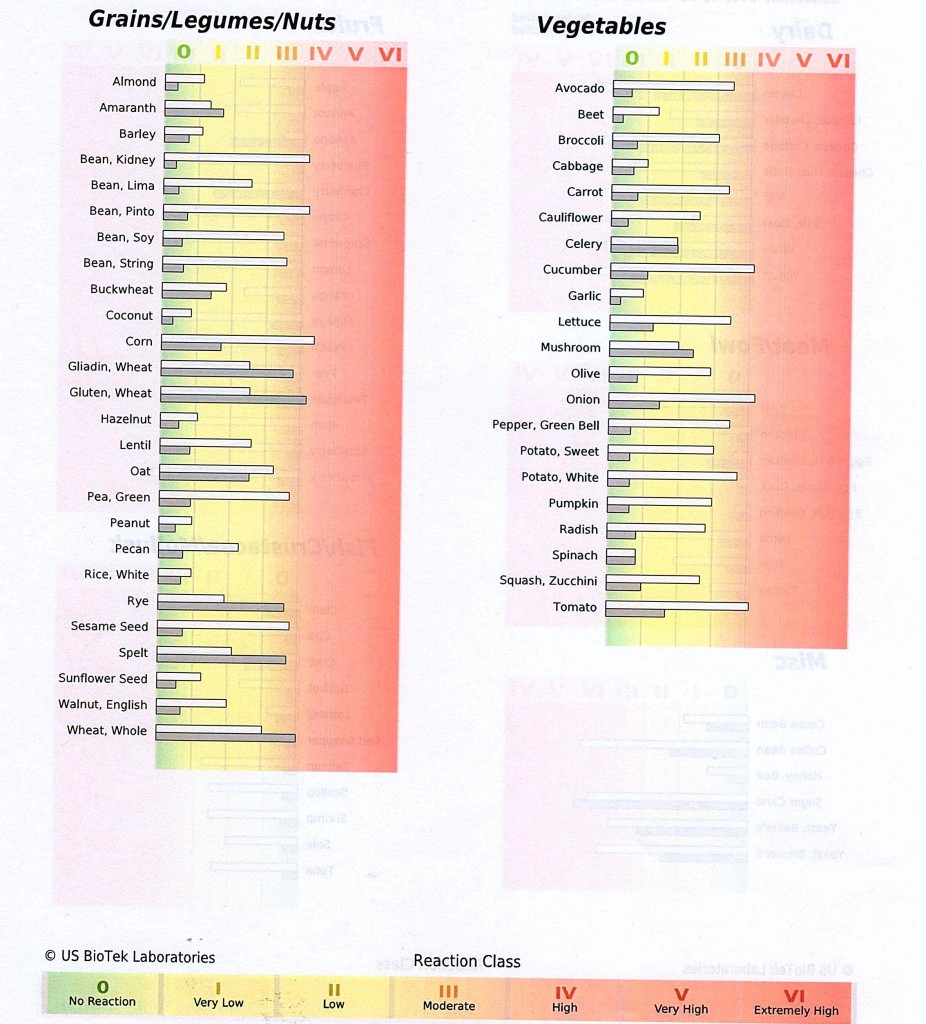
Another example IgG & IgA antibody test







Hi Maria,
Like Andrew I would like to know where to begin to find out my daughter’s possible food intolerances. I live in Mt Helena Western Australia
Megan
So what’s the first port of call for testing, GP or Naturopath ?
Hi Andrew,
GPs don’t test for intolerances I’m afraid, although you can get Total IgA and IgG (as well as IgE) through a GP to see if the total numbers are elevated, then dig deeper into individual foods with nutritionist/naturopath. I can recommend someone in your area if you send me an email through the contact page on the website.
Cheers,
Maria